Surgical Specialities
Dr. Emile Woo
General Surgeon

Dr. Emile Woo is a General and Head & Neck Surgeon. He is a Clinical Associate Professor at the University of British Columbia. He is also dedicated in training new surgeons and was the residency coordinator for Mount Saint Joseph Hospital and former Chair of the Competency Based Medical Education Committee. He is also a member of the BC Cancer Agency's GI Tumor Group. He currently also serves as the President of the Medical Staff at Providence Healthcare (St. Paul’s and Mount Saint Joseph Hospitals)
Dr. Woo received his medical degree at the University of British Columbia. He went on to complete a residency in General Surgery at McMaster University followed by additional sub-specialty training in Head and Neck surgery. He has also worked in Singapore and was involved in teaching residents there as well. He has also lectured and has been invited to speak in Canada and Internationally on topics such as Geriatric Surgery and Gastric Cancer. He is one of the Co- Authors of the BC Provincial Guidelines for the management of Gastric Cancer. He continues to be active in research in the area of Gastric Cancer as well as Perioperative Safety for patients. He will also be the Conference President and Host for the 2028 Asia Pacific Gastroesophageal Cancer Congress here in Vancouver
Treatments and Surgeries
- Capsule Colonoscopy - returning Spring 2025
- Gastroscopy and Colonoscopy
- Gastric Cancer Screening
- Colorectal Cancer Screening
- Hernia Treatment
- Rectal Bleeding
- Hemorrhoids and Treatment
- Gallbladder Disease: Stones, Polyps, and Cancer
- Thyroid Nodules
- US Guided Needle Biopsy - Thyroid
- Laser Hemorrhoid Treatment - Coming Soon
Capsule Endoscopy
Visualization of the Colon without an invasive procedure!
Many people know that a colonoscopy is the gold standard test for colon cancer screening. However, there are legitimate concerns as the procedure is invasive and has a risk of causing an injury or perforation of the colon. As well, sedation of some form is required for most patients to be able to tolerate the procedure.
However, there is now an alternative that will allow for visualization of the colon without the need for an endoscope. As well, unlike CT colonography, this new method does not require any radiation dose and is able to show actual pictures of the colon instead of black and white digital ones. Colon Capsule is currently being used in the UK for primary screening for colon cancer.
PillCam Colon2 is a capsule with two cameras on either end that can capture up to 30 images per second. It then sends the pictures to a recording device that is comfortably worn by the patient. Once the study is complete, it is uploaded to a computer and the images are analyzed by one of our specialist doctors.
Patients do require a bowel cleanse prior to the study to allow the capsule to see clearly. However, there is no sedation required, no risk of perforation, and no radiation. There is a small risk of a retained capsule in 1% of patients. There is also a small risk of incompletely seeing the colon if the patient’s bowels move slowly.
If you are interested in seeing if PillCam Colon2 is appropriate for you, contact us today.
Gastroscopy and Colonoscopy
The best method of examining the stomach and the large intestine is using a flexible endoscope. At the end of the endoscope, there are bright LED lights and a camera system that allows for high definition images to be seen and recorded. Within the endoscope are channels that allow for suction and also placement of small instruments to allow for biopsy and removal of tissue, such as polyps.
Gastroscopy is used to examine the stomach. It is used to assess patients with stomach pains and can evaluate ulcers, stomach polyps, acid-reflux disease, as well as gastric cancer.
Colonoscopy is the gold standard for examining the large intestine for colon cancer. It is also used to assess patients for inflammation and bleeding. Colonoscopy does require a bowel cleanse in order to clearly see the colon. This is usually performed the day before.
Endoscopy is a very common and safe procedure. However, there are small risks associated with endoscopy. For colonoscopy, there is a small risk of causing an injury or perforation of the large intestine that can usually be treated without surgery. There is also a small 1% chance that, if the large intestine is very tortuous or long, it may not be able to see the entire colon. Lastly, there is a small risk of missing a small cancer in 1% of patients.
With both gastroscopy and colonoscopy, some sort of sedation is required to make the procedure comfortable for patients. At PEH, we can arrange for Gastroscopy and Colonoscopy in a timely manner. We can arrange for this either at a private office facility that offers IV sedation or at a private surgical facility that includes an anesthetist who can offer completely pain free endoscopy with what is similar to a general anesthetic.
Gastric Cancer Screening
Barium swallow is considered an older technology for gastric cancer screening. The way it works is that the patient drinks an X-ray dye that coats the stomach. Then x-rays are taken that shows the stomach in outline (Figure 1). The radiologist then looks at this indirect outline of the stomach to look for growths or ulcers.

Figure 1: Barium Swallow outline of the stomach
Gastroscopy, though more invasive, allows one to look directly at the lining of the stomach. For this reason, we can see even early changes that are not visible on the barium swallow. There has to be a larger structural change to be seen on barium swallow - it can’t see early changes that may show up only as just an abnormal discolouration with very little physical change (Figure 2). This can only be seen on gastroscopy as we can look much more closely and can even add different filers to highlight changes. The cancer in the figure is very subtle.

Figure 2: Early gastric cancer on endoscopy under different filtered light.
So, gastroscopy will be able to detect earlier changes so that we can either, prevent change to cancer, or catch cancer early. As well, if there is are changes, we can immediately biopsy the area. It is superior to barium swallow.
What is important as well is that there are very few people trained to detect early gastric cancer in Canada as it is seldom seen here. The quality of barium swallow here is not as good as in Japan (it is rather poor outside of hospitals). Even in hospital, the radiologists are not trained to do gastric cancer screening.
Catching gastric cancer early is extremely important. The earlier it is caught, the better the outcome. That is one of the reasons why it is much better treated in Japan - it is caught early, In the US and Canada, most of the cases are found late. If you look at Figure 3, you can see 53% of cases in Japan are early (Localized), whereas in the US (and Canada), it is only 27%. Most are discovered to already have regional spread or distant spread.
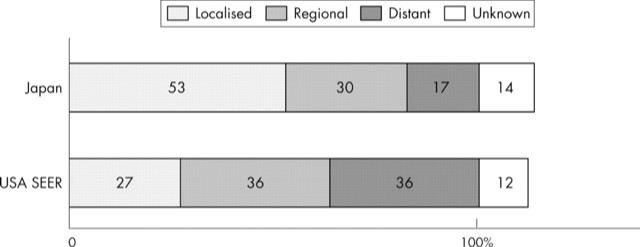
Figure 3: distribution of gastric cancer cases in Japan vs. US
For especially the Japanese and Korean clients, it is very important to have screening done by doctors trained to deal with gastric cancer. Dr Woo is one of the few Vancouver based Surgeons with a training in gastric cancer.
Colorectal Cancer Screening
What is colorectal cancer?
Colorectal cancer is cancer that arises from the inner lining (mucosa) of the large intestine and the rectum. In Canada, colorectal cancer is the third most common cancer and is the second most common cause of cancer death. As Asian countries have become developed and adopt a more Western style diet, the rates of colorectal cancer have risen and are approaching Western rates. As you can see in the tables below, the rate of colorectal cancer in China is steadily increasing in both males and females. (Figures taken from Chen, W et. al., 2015, CA)
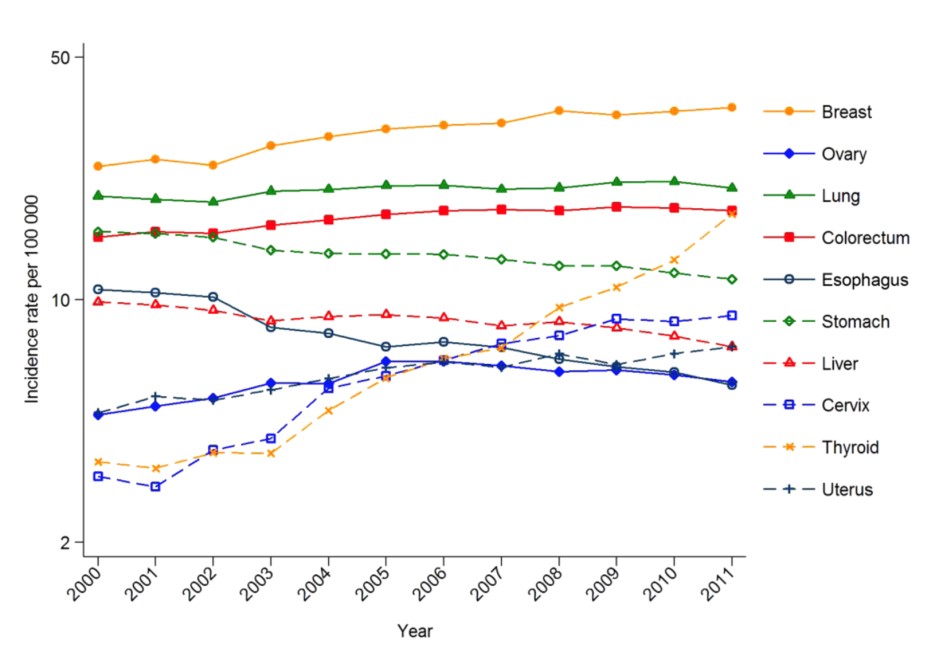 Figure 1: Rates of Cancer in Females in China (2000-2011)
Figure 1: Rates of Cancer in Females in China (2000-2011)
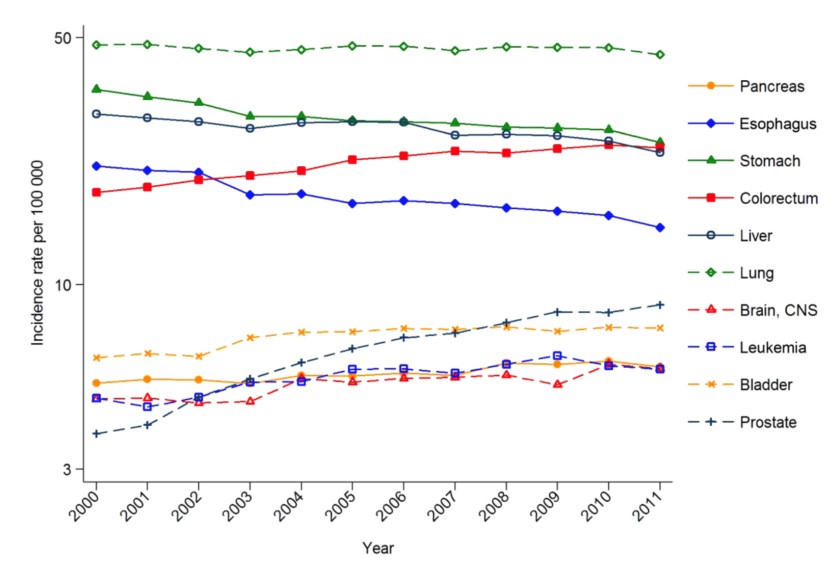 Figure 2: Rates of Cancer in Males in China (2000-2011)
Figure 2: Rates of Cancer in Males in China (2000-2011)
Why do screening?
Unfortunately, like most cancer, colorectal cancer in its early stages are usually asymptomatic; that is, they have no symptoms whatsoever. As the cancer enlarges, it can cause:
Bleeding
Alterations in the bowel pattern
Unexplained weight loss
Unexplained anemia
However, these symptoms usually do not occur until the cancer is more advanced. Therefore screening, that is, testing patients without symptoms, is the best way to try to detect for colorectal cancer. As well, colorectal cancers usually arise out of small growths on the inner lining of the intestine call polyps. Screening can detect for these polyps. Removal of these polyps may then prevent future cancer.
Who should be screened?
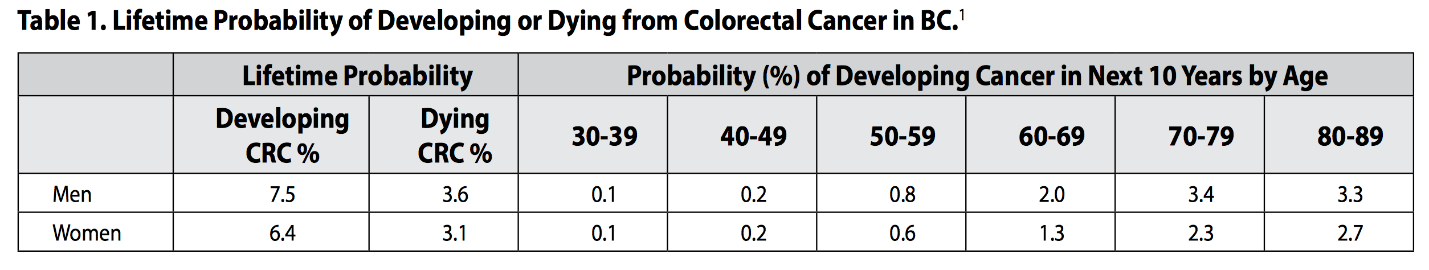
The biggest risk factor for colorectal cancer is age. The risk of cancer steadily rises with increasing age as can be seen in Table 1.
What methods are there to do screening?
FIT Test / Stool Test
Currently, the Provincial government recommends stool testing using a FIT test for initial screening for patients who are over 50 with no family history of either a first degree relative under 60 or 2 first degree relatives.
FIT testing is used to detect for the presence of abnormal amounts of blood in the intestines that may be due to a cancer or large polyps. FIT testing is very safe and does not require any preparation of the intestines. A positive FIT test requires a colonoscopy to confirm if there is a cancer or polyps. A FIT test can miss a cancer or large polyp in around 5% of patients. It cannot detect for early or smaller polyps.
Colonoscopy
Colonoscopy is considered the gold standard for screening by most Surgeons and Physician groups. It is also recommended for patients with a family history of colorectal cancer in a first degree relative under 60 or two first degree relatives. It utilizes a long, flexible tube with a camera at the end to allow for visualization of the entire colon.
Colonoscopy picks up 99% of all cancers. It is also able to perform biopsies as well as removal of polyps at the same time. However, it does require preparation of the bowel with cleansing. It also requires IV sedation as it can cause pain. Lastly, there is a known risk of causing an injury or perforation of the colon in 1:1000 patients with a mortality risk of 1:10000. The risk appears to increase with age.
PillCam Colo2- Capsule endoscopy
Capsule endoscopy is a newer technology whereby a patient swallows a capsule that has a camera on both ends and allows for complete visualization of the colon and rectum. It is considered an alternative to colonoscopy for patients unwilling or who are concerned about the risk of perforation.
Capsule endoscopy does require a full bowel preparation but does not require sedation. There is no risk of perforation. There is a small 1% risk of a retained capsule as well. If an abnormality is found, colonoscopy may be required for biopsy. Capsule endoscopy may not see abnormalities smaller than 5-6mm.
CT Colonography
CT colonography is a specialized CT scan that focusses on the intestines. It is considered an alternative to colonoscopy. In this test, patients also require a bowel preparation to cleanse the intestines and also need to drink some x-ray contrast to coat the lining of the intestine. During the test, CO2 is pumped into the colon via the anus and then a CT scan is performed.
CT colonography does have a small risk perforation due to the need for CO2 inflation. As well, it cannot see abnormalities under 6mm. Lastly, the images are only computer generated and thus do not have color and hence, inflammation cannot be reliably assessed.
Do you need colon screening or want to ask about the various methods available? At Pacific Executive Health, we can offer the full range of screening methods.
Hernia Treatment
What is a hernia?
Hernias occur when there is an abnormal protrusion of an organ into an area where it usually is not supposed to be. The most common hernia is what is called an inguinal hernia. These are due to a tear or disruption of the strength layer of the abdominal wall in the groin. Normally, the muscles and fascia of the deeper layers of the abdominal wall provides strength and holds the abdominal organs inside. In a hernia, there is essentially a hole in the muscle and fascia layer such that the organs inside the abdominal cavity (such as the intestines) now protrude outwards under the skin. Other hernia types include femoral as well as incisional hernias.
What happens if the hernia is not repaired?
Over time, the hole will enlarge and more of the internal organs will push out and therefore the hernia will become larger. How quickly this happens is unpredictable. As the hernia enlarges, it can become more painful and inconvenient. Many patients with hernias are unable to exercise or may have lots of pain with prolonged standing or walking.
The most concerning aspect of a hernia is the risk of what is called incarceration or strangulation of a hernia. This is when one of the internal organs, such as the intestine, comes through the defect/hole in the abdominal wall and gets trapped or twisted and cannot be reduced/pushed back into the abdominal cavity. If this happens, it can be an emergency. Usually, patients will feel sudden, severe pain at the bulge of the hernia and may feel nauseated or vomit. This needs to be treated within 6 hours or else the portion that is trapped outside may become gangrenous.
How are hernias repaired?
Hernias can only be repaired using surgery. There are no exercises or medications that can be used to close the hole. In the short term, patients with symptoms can purchase a hernia belt to try to hold in the hernia and prevent symptoms.
Surgery involves reducing all of the organs that have come out back into the abdomen and then repairing the hole by placing a mesh made of a plastic polymer to patch the whole. The surgery can be done using either a small 5 to 7cm incision in the traditional way or via 3 small openings using a laparoscopic technique. Surgery usually is requires under one hour and patients may go home the same day.
If you have a hernia, Pacific Executive Health can arrange a rapid assessment with Dr. Emile Woo. We also have access to private surgical facilities so that you will not have to wait for months to have your hernia repaired while you are suffering from pain and unable enjoy the activities you want to do. Dr. Woo has performed thousands of hernia surgeries and can perform both traditional open surgery as well as advanced Laparoscopic surgery.
Rectal Bleeding
Rectal bleeding is a very common condition. However, seeing blood in the toilet can be a very frightening experience as even a small amount of blood can stain the water very red.
The vast majority of patients who experience rectal bleeding do not have anything ominous or worrisome. However, even just one episode of rectal bleeding should require an assessment with a doctor to confirm that it is due to a benign reason.
The most common causes of rectal bleeding are:
- Bleeding internal hemorrhoids
- Anal Fissures
- Anal Fistulas
More serious causes of rectal bleeding are:
- Colon or rectal cancer
- Bleeding from diverticular disease
- Inflammatory bowel disease
- Food poisoning
Many people are concerned about the risk of colorectal cancer. Patients that have the following symptoms along with their bleeding may require a colonoscopy to be sure:
- Blood that is mixed into the stools
- Blood that is dark (not bright red) or there are clots
- Altered bowel patterns
- Unexplained weight loss
- New onset urgency with having a stool
- A family history of colorectal cancer in a first degree relative
If you have lots of bleeding, you should go to your nearest Emergency Department.
At Pacific Executive Health, we can arrange for a rapid Assessment including a same day scope of the anus and rectum for diagnosis of hemorrhoids, fissures, inflammation, as well as rectal cancers. We can also schedule private screening using colonoscopy or pillCam Colon if required. Treatment of your hemorrhoids can be provided as well.
Hemorrhoids and Treatment
What are hemorrhoids?
Hemorrhoids are normal cushions of tissue that are situated around the anal canal. They help with the normal opening and closing of the anal sphincter. Everyone has hemorrhoids. However, when people speak of having hemorrhoid problems, it usually refers to the fact that they have enlarged and can bleeding, prolapse, or become swollen and painful.
Hemorrhoids are divided into either External or Internal Hemorrhoids.
Internal hemorrhoids are found within the anal canal and are normally not seen. When internal hemorrhoids enlarge, they can either bleed or prolapse out. Internal hemorrhoids, as they are internal, normally do not have any nerve endings and therefore do not have any sensation. Most people will have painless, bright red blood when they bleed. If they prolapse, patients may feel a sense of some tissue coming out. If the hemorrhoid is not very large, it will usually reduce, that is, go back inside, on their own. If it is larger, patients may have to use their hand to push it back in.
Normally, treatment of internal hemorrhoids does not require surgery anymore. They are usually quite easy to treat by either injecting them with a medication that causes the hemorrhoid to shrink or shrivel up. Another common way of treating hemorrhoids involved placing a small rubber band across the base of the hemorrhoid. This will then cause the hemorrhoid to fall off over a few days. Surgery is only required for very large hemorrhoids.
External hemorrhoids are found on the outside of the anus. They show up as bulges of tissue that look like grapes or may be flat like the petals of a flower. Normally, external hemorrhoids are not symptomatic and are very common. However, in a small number of patients, they may become swollen and inflamed. This can be extremely painful. External hemorrhoids, as they are covered by skin, are very sensitive and can only be treated with surgery and usually requires a general anesthetic.
If you have hemorrhoids, Pacific Executive Health can arrange for a rapid assessment so that you can be diagnosed and treated quickly.
Gallbladder Disease: Stones, Polyps, and Cancer
What is the Gallbladder?
The gallbladder is a storage organ for bile. Bile is required to help you digest fats in your food. It helps to emulsify the fat into water so that your body can absorb it. Bile is not made in the gallbladder but is made in the liver.
Gallstones
Gallstones are very common in the normal population. In North America, the number of people who have gallstones is between 10-15%. It may be as high as 50% in some groups of people such as Aboriginal Canadians. Asians also tend to have higher rates of stones and usually have different types of stones from Caucasians. Caucasians tend to have cholesterol stones whereas Asians tend to have pigmented stones that are black or brown.
Most patients (80%) who have gallstones do not have any symptoms. Only a small minority do. The typical symptoms are:
Pain after eating fatty foods
Pain that is severe and constant
Pain that is in the epigastric/upper mid abdomen or to the RIGHT, just under the rib-cage
With a severe attack, the pain can go into the back and into the shoulders
Surgery is the only definitive cure for patients who have gallbladder symptoms. The preferred method is to remove the gallbladder using laparoscopic surgery using 4 small incisions.
Gallbladder Polyps
Gallbladder polyps are very common. The vast majority of polyps are small, and benign. They are usually made up of cholesterol that has become attached to the gallbladder wall and the appearance, on ultrasound, shows a polyp like growth. However, gallbladder polyps that are greater than 1cm are associated with a risk of cancer and laparoscopic surgery is recommended to prevent cancer.
Gallbladder Cancer
Gallbladder cancer is very rare in North America. However, gallbladder cancer is very difficult to treat as the gallbladder is very thin and therefore cancer spread occurs very easily. As well, there are some places where gallbladder cancer is more common, such as in Shanghai, China. Symptoms of gallbladder cancer is usually very vague and occurs late. The only proven method of treatment is early diagnosis and surgical removal of the gallbladder.
If you have a gallbladder problem, Pacific Executive Health can arrange for a rapid assessment with one of our experienced surgeons. We can also arrange for private surgery with the long wait that is usual in the public system.
Thyroid Nodules
What is the thyroid?
The thyroid is a small, butterfly-shaped organ that is located at the base of the neck. It is responsible for secreting Thyroid Hormones which are responsible for regulating your bodies metabolic rate.
What are thyroid nodules?
Thyroid nodules are abnormal growths within the thyroid itself. Nodules are very common in women with up to 50% of women having nodules by the age of 50. Around 95% of nodules are benign/non cancerous. The may be caused by hormonal changes, family history, as well as certain dietary factors.
How do you know if my nodule is benign or cancerous?
There are a number of risk factors for thyroid cancer. These include radiation exposure at childhood, being of child bearing age, certain countries have a higher risk of thyroid cancer such as in China where there is a rising incidence, as well as family history for thyroid cancer.
The most important test to know whether a nodule is benign or not is via a Fine Needle Aspiration. In this test, a small needle is inserted into the nodule and cells are taken out and sent to a lab for analysis. The procedure can be done in the office and usually takes under 10 minutes. A result will usually come back in under 1 to 2 weeks.
At Pacific Executive Health, we can arrange for a rapid Assessment with our experienced thyroid surgeon. We may be able to perform a biopsy for you on the same day. Contact us if you have any questions.
US Guided Needle Biopsy - Thyroid
Starting in 2025, our surgeon will be offering Private US guided Fine Needle Aspiration for Thyroid nodules.
-accurate localization of thyroid nodules
-simple, 5 to 10 min procedure without the need for anesthesia
-98% accuracy in determining the type of nodule (all samples are sent to expert cytologists for interpretation)
-we can arrange to have this done within 2 to 3 weeks (vs 6 months or more in the public system)
-if you require surgery, our surgeon can arrange for expedited surgery
For patients who do not have BC MSP, before we can perform a biopsy, we require:
1. Your Thyroid Ultrasound showing which nodule(s) require biopsy
2. A virtual consultation with our surgeon
For patients with BC MSP, you will require:
1. a referral from your Primary Care Provider to Dr. Emile Woo
2. Your Thyroid Ultrasound showing which nodule(s) require biopsy
3. An in person or Virtual consultation with our surgeon
